Dental FAQs – Answers to Your Questions
Answers to Your Dental Questions – Helping You Make Informed Decisions
Got questions about your teeth or a visit to the dentist? We’re here to help.
Whether you’re wondering how to keep your teeth in top shape, how your oral health links to the rest of your body, or what happens during an x-ray, we’ve got the answers.
If you’re unsure about something or feeling a bit nervous, just get in touch. Our friendly team is happy to chat and help put your mind at ease.
Artificial Heart Valves and Oral Health
Infective Endocarditis
Infective Endocarditis is a serious infection of the inner lining of the heart or heart valves. It’s usually caused by bacteria entering the bloodstream and settling on damaged areas of the heart. Once there, it’s hard for the body to fight off.
How does this relate to dental care?
Bacteria from the mouth can sometimes enter the bloodstream—especially if you have gum disease, an untreated dental infection, or during certain dental procedures. This is why good oral hygiene is so important, especially if you’re at higher risk.
Who’s at risk?
If you have an artificial heart valve, a history of rheumatic fever, or other heart valve problems, you may be more likely to develop this infection. In some cases, your doctor or dentist might recommend a short course of antibiotics before certain treatments to lower the risk.
Not sure if this applies to you? Chat to your GP, dentist, or specialist—they’ll help you decide what’s best for your health.
For more information, visit the Heart Foundation’s page on Infective Endocarditis.
Artificial Joints
If you’ve had a joint replacement (like a hip or knee) within the last 2 years, there’s a small risk that oral bacteria could affect the joint. Some people may need antibiotics before dental treatment as a precaution. Not everyone does—so it’s best to talk it through with your dentist or hygienist.
Brushing and flossing
 At Dental Solutions, we like to keep things simple:
At Dental Solutions, we like to keep things simple:
Only floss the teeth you want to keep!
You don’t have to be perfect—just consistent. Here’s how to look after your smile at home.
Flossing
Floss once a day—whenever suits you best. If you’re just starting out, your gums might bleed a bit. That’s actually a sign they need a little extra love. Stick with it, and it will get better.
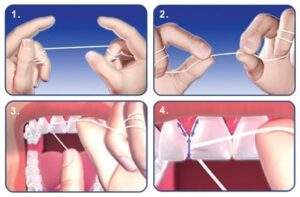
How to floss properly:
- Take about 45cm of floss and wrap most of it around your middle fingers
- Hold the floss tight between your thumbs and fingers
- Gently slide it between your teeth
- Curve it around each tooth and go just under the gumline
- Use a fresh bit of floss as you move from tooth to tooth
Brushing
Brush twice a day for two minutes using fluoride toothpaste. Gentle is best—scrubbing too hard can damage your gums.
Top tips for brushing:
- Use a soft-bristled brush (or electric)
- Divide your mouth into four sections—30 seconds each
- Hold the brush at a 45° angle to the gumline
- Use gentle circles or short strokes, not hard scrubbing
- Don’t forget behind your front teeth—hold the brush upright for these
- Brush your tongue too—it helps with breath
- Spit, but don’t rinse. Let the fluoride work its magic
For Kids
Start brushing as soon as their first tooth comes through. Use a super-soft brush made for little mouths. And don’t worry—most kids go through a “brushing is boring” phase. You’re not alone. Keep at it and guide them through.
Which Toothbrush Should I Use?
Soft bristles are always best. Manual or electric? Up to you. Both work well if used correctly, but electric brushes often make it easier to get a good clean.
And remember: swap your toothbrush (or head) every 3 months—or sooner if it’s looking a bit tired.
Diabetes and Oral Health
If you have type 1 or type 2 diabetes, your oral health needs a bit of extra care. Unfortunately, it’s a bit of a cycle—poorly controlled blood sugar can lead to dental problems, and dental problems can make it harder to manage your blood sugar. But the good news is that with a few simple steps, you can stay on top of both.
Common dental issues for people with diabetes include:
- Gum disease
- Fungal infections (like thrush)
- Dry mouth (xerostomia)
Before Your Appointment
Here’s what to keep in mind if you’re visiting the dentist or hygienist:
- Let us know if you have diabetes, and keep us updated on any medications you’re taking
- Eat before your appointment so your blood sugar is stable
- If you’re on insulin, morning appointments after a normal breakfast are usually best
We’re here to help make your visit smooth and safe. If you have any questions, just ask—we’re always happy to talk it through.
Dry Mouth (Xerostomia)
Dry mouth isn’t just uncomfortable—it can also lead to more tooth decay, gum disease, and bad breath. If you’re dealing with it, you’re not alone, and there are ways to manage it.
Simple tips that can help:
- Sip water regularly—carrying a water bottle can be a game-changer
- Sugar-free chewing gum can help boost saliva flow for a short while
- We also stock dry-mouth gels that are specially designed to mimic saliva and provide longer-lasting relief
If dry mouth is bothering you, chat to our team. We can help you find the right solution for comfort and long-term care.
Fluoride – And Why It Matters
Tooth enamel is made up of tiny crystals that band together to form the super tough outer layer of your teeth. But here’s the tricky part—those crystals start to dissolve when acids from plaque or acidic food and drinks hit your teeth. That’s called demineralisation, and it’s how cavities get started.
Unlike most parts of your body, tooth enamel can’t repair itself once it’s damaged. That’s where fluoride steps in.
Fluoride is a natural mineral that helps rebuild and strengthen enamel. It soaks into your teeth and draws in other useful minerals from your saliva—a process called remineralisation. This helps make your enamel stronger and more resistant to decay.
Your mouth is constantly swinging between demineralisation and remineralisation.
- When you eat or drink, your mouth becomes acidic → enamel starts to weaken
- When you stop eating and the acid levels drop → enamel can start to rebuild
The problem? If you’re snacking often or sipping sugary drinks throughout the day, your mouth stays acidic—and your teeth don’t get the chance to recover.
If you’re getting cavities more often than usual, it could be a sign that you’re not getting enough fluoride. Our clinical team is always happy to chat and help figure out what’s going on. There are a few treatment options available, and we’ll work with you to find something that suits your needs and budget.
Heart (Cardiovascular) Disease and Oral Health
The Gum Disease and Cardiovascular Disease Link
Infective Endocarditis-
How do I reduce the risk?
Always tell your dentist and hygienist if you are on any medications.
Pregnancy & Your Oral Health
First things first—congratulations! Pregnancy is a special time, but it’s also an important time for looking after your oral health. Your body goes through a lot of changes, and your teeth and gums feel it too.
Should I Still See the Dentist While Pregnant?
Yes—definitely. Hormone changes, morning sickness, and changing eating habits can all affect your mouth. Regular check-ups help catch any issues early and keep you feeling your best. If you’re pregnant or think you might be, just let us know so we can tailor your care.
Morning Sickness & Tooth Erosion
If you’re dealing with morning sickness, you’re not alone. Unfortunately, vomiting exposes your teeth to stomach acid, which can weaken the enamel.
Important tip:
After vomiting, don’t brush your teeth straight away—it can damage the softened enamel. Instead, rinse your mouth with water or a fluoride mouthwash. Wait at least 30 minutes before brushing to give your enamel time to recover.
Pregnancy Gingivitis
Many mums-to-be notice their gums becoming red, swollen, or prone to bleeding—this is called pregnancy gingivitis. It’s caused by higher levels of progesterone and estrogen, which increase blood flow and make the gums more sensitive to plaque and bacteria.
The best way to keep things under control is to:
- Brush twice a day
- Floss daily
- Visit your hygienist for gentle, professional cleaning
Pregnancy Granuloma
Occasionally, pregnant women can develop a pregnancy granuloma—a small, red or purple growth on the gums, usually between the teeth. They’re often harmless and shrink after baby is born, but if one becomes painful or troublesome, your dentist can help.
What About X-Rays?
If x-rays aren’t urgent, we’ll hold off until after baby arrives. If one is needed, we use a lead apron to protect your bump and keep things safe.
We’re Here to Support You
Pregnancy can bring all kinds of surprises—dental included! Our clinical team is here to make things as easy and comfortable as possible. If you’ve got questions or concerns, just give us a call. We’re always happy to help.
Why are My Teeth Sensitive?
That sharp twinge you get when enjoying a hot drink, a cold snack, or even while brushing? It’s often a sign that the dentine under your enamel has become exposed.
Dentine is the softer, yellowish layer beneath the enamel. It’s packed with tiny tubules that lead straight to the nerve inside your tooth. When those tubules are exposed—often due to gum recession or worn enamel—things like heat, cold, sweetness, or pressure can set off that quick burst of pain.
What You Can Do
Sensitivity can come and go, and many people find relief by simply switching to a sensitive toothpaste. But if the pain lingers or starts getting worse, don’t brush it off—it could be a sign of a bigger issue.
We have in-chair treatments available that can protect those exposed areas and help calm things down. Just let us know at your next visit, and we’ll talk you through the best options.
Got questions? Let us know at your next visit—we’ll help you find what works best for your teeth.
Smoking & Oral Health: What You Need to Know
Most people know smoking harms overall health—but it also takes a serious toll on your teeth and gums.
If you smoke, you may have already noticed some of these effects:
- Yellow or brown staining on your teeth
- Persistent bad breath
- A reduced sense of taste and smell
- Buildup of tartar (calculus)
- Receding gums and gum disease
- Tooth loss
- In more serious cases, oral cancer
Why Is Smoking So Harmful to Your Mouth?
Smoking reduces blood flow to your gums, depriving them of the oxygen and nutrients they need to stay healthy. This makes your gums more vulnerable to infection and slows healing after dental treatments.
Smokers are not only more likely to develop gum disease—a leading cause of tooth loss—but they’re also three times more likely to develop oral cancers than non-smokers.
Thinking About Quitting?
If you’re ready to quit or just want to explore your options, have a chat with the team. We’re here to support you with advice, encouragement, and helpful tools to get you started.
Tooth Erosion
Tooth erosion is when the hard outer layer of your teeth—called enamel—wears away. Enamel protects the softer, more sensitive layer underneath. Once it’s gone, you might feel pain or sensitivity, especially with cold, hot, or acidic things (see also Why are my Teeth Sensitive).
Erosion usually happens slowly over time, so it’s easy to miss. You might notice hollows on your back teeth, or that your teeth look a bit thinner, smaller, or more yellow. That’s the dentine showing through.
Tips to help protect your enamel:
- Try not to snack on acidic food and drinks too often
- Don’t swish drinks around your mouth
- End meals with a bit of cheese or milk—it helps balance out acids
- Wait at least an hour after anything acidic before brushing your teeth
Wisdom Teeth
Wisdom teeth are your third molars—the ones right at the back. They usually show up in your late teens or twenties, though some people get them later. And some people never get them at all!
How do wisdom teeth cause trouble?
Often there’s not enough room for them to come through properly. When that happens, they can:
- Get stuck under the gum (impacted)
- Only come through partway, making them hard to clean
- Cause infections, swelling, or bad breath
- Push against other teeth or cause crowding
- In rare cases, lead to cysts or damage nearby teeth
Do they always need to be removed?
Not necessarily. We only recommend removing wisdom teeth if they’re causing problems or likely to in the future.
What happens if I need them out?
Your dentist will take an x-ray to check what’s going on. If the removal looks straightforward, we can do it here at the practice. If it’s more complex, we’ll refer you to a specialist oral surgeon and talk you through the next steps.
Why Do I Need X-Rays?
X-rays help your dentist spot problems that aren’t always visible during a regular check-up. They can show hidden decay, check old fillings, and help assess the bone around your teeth.
Are dental x-rays safe?
Yes—they’re very safe. The amount of radiation is tiny, much less than what you’re exposed to naturally from the sun or everyday devices. We usually avoid x-rays during pregnancy, just to be cautious, but otherwise they’re a routine part of good dental care.
Posterior Bite-Wing X-Rays (PBWs)
Bite-wing x-rays are a routine part of most check-ups. They show your back teeth—from premolars to molars—and help us spot any decay between the teeth, check on old fillings, and keep an eye on bone levels.
We usually take them once a year to make sure everything’s healthy and nothing’s hiding out of sight.
Panoramic X-Rays

A panoramic x-ray gives us a full view of your mouth, jaw, sinuses, and surrounding areas—all in one image. It helps us spot things that aren’t always visible in smaller x-rays, like cysts, bone changes, or hidden issues in the jaw joints and sinuses.
We usually recommend having a panoramic x-ray every 5 years as part of a routine screening for anything developing beneath the surface.
Got Questions? We’re Here to Help
If you’ve got concerns or just want to chat about your dental health, our friendly team in Tauranga is here for you.
We understand that one size doesn’t fit all. Everyone’s needs—and nerves—are different. If you’re feeling anxious about visiting the dentist, you’re not alone. At Dental Solutions, we treat every patient the way we’d want to be treated ourselves—with kindness, honesty, and care. Our relaxed and caring approach is all about helping you feel comfortable, informed, and confident at every step.
Ready to get started?
Give us a call or email to book your first check-up—we’d love to welcome you to the practice.
